
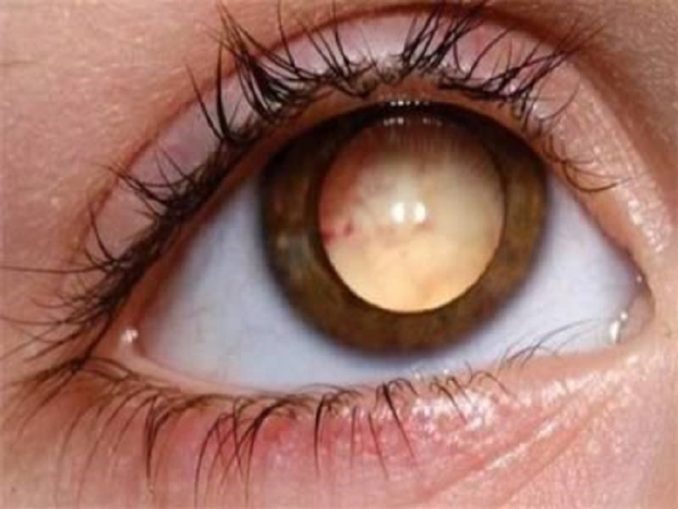

Bull's eye-maculopathy seen on FAF and IS/OS irregularities seen on SD-OCT. Prolonged use of the chloroquine derivatives typically results in a pigmentary maculopathy. Today, they are more commonly used to treat autoimmune conditions such as rheumatoid arthritis or systemic lupus erythematosus. Other forms of toxicity can also include serous retinal detachments ( MEK inhibitors, FGFR inhibitors) and retinal edema and atrophy ( quinine).Ĭhloroquine and its derivative, hydroxychloroquine sulfate, were initially used as malarial prophylaxis. Medications that can induce a pigmentary maculopathy include chloroquine derivatives (chloroquine, hydroxychloroquine), phenothiazines (thioridazine, chlorpromazine), pentosan polysulfate sodium, clofazimine, dideoxyinosine, deferoxamine, ritonavir, alkylating agents (cisplatin, BCNU), potassium or sodium iodate, and denileuken diftitiox. The most common manifestation of injury to the retina and RPE is a pigmentary maculopathy. Disruption of retina and pigment epitheliumĭrugs can be directly toxic to the cells of the retina or the retinal pigment epithelium (RPE). This table presents a brief overview of drug-induced retinal toxicities and the pattern of injury typically associated with each drug.ĭisruption of the retina and retinal pigment epitheliumĪdapted from Zhu I, Andreoli MT, Mittra RA, et al. Retinal drug toxicities can manifest in a variety of patterns. 3.2 Aminoglycoside antibiotics (intraocular).2 Disruption of retina and pigment epithelium.


 0 kommentar(er)
0 kommentar(er)
